The typical symptom of all types of pulmonary edema is the sensation of shortness of breath, or dyspnea, the severity of which depends on the causes that have caused the condition and which must be identified as soon as possible.
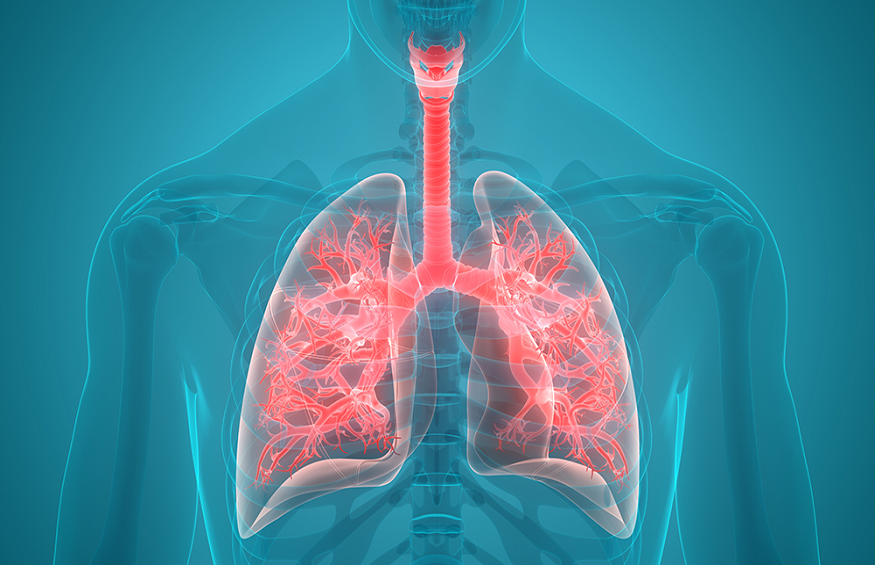
It is called pulmonary edema to the accumulation of fluid inside the lungs. If it occurs in a short period, it is usually called acute lung edema. In this case, it is a medical emergency since the patient’s respiratory capacity may be compromised.
Table of Contents
Why happens? Causes of pulmonary edema
The lungs fill with fluid when the blood that is usually inside the blood vessels flows to the outside, flooding the pulmonary alveoli. Of course, this only happens when something goes wrong in the lungs or the heart; Thus, we can divide lung edema into the following types:
- Cardiogenic lung edema
- Non-cardiogenic lung edema
- Neurogenic pulmonary edema
They all have in common that they cause a sensation of shortness of breath, also known as dyspnea.
The most common cause of pulmonary edema is usually congestive heart failure, which in turn can be caused by a sudden rise in blood pressure, aortic valves, or heart attacks, or myocardial problems.
However, pulmonary edema can also be due to other causes, such as taking certain drugs, kidney failure, lung damage caused by poisoning or infections, being exposed to high altitudes.
Types of pulmonary edema
We could say that there are various types of pulmonary edema, which depending on their production mechanism, we could divide into two large groups: cardiogenic and non-cardiogenic. Although there are also other less frequent forms. Let’s see them in more detail:
Cardiogenic lung edema
To understand this type of edema, it is necessary to remember the blood circulation. The heart receives blood from the whole body in the right atrium, and from there, it passes to the right ventricle, which pushes it to the lungs to oxygenate the blood. Afterward, all the blood from the lungs is collected in the left atrium and passes through the mitral valve to the left ventricle, propelled to the rest of the human body.
Any disease that causes a malfunction of the left part of the heart will cause blood to pool backward, that is, towards the lungs, which is where it stagnates. This malfunction is known as left heart failure (the heart’s left side is not efficient enough to pump all the blood it needs). The situations in which left heart failure occurs are:
Acute myocardial infarction: when part of the heart muscle is destroyed, the heart loses pumping power. The severity of this loss of efficacy depends on the extent of the infarcted area.
Cardiac arrhythmias: the heart loses the proper pumping rhythm, and blood is not appropriately expelled.
Mitral stenosis: A narrowing of the mitral valve would make it more difficult for blood to flow from the left atrium to the left ventricle.
Mitral rupture: if the mitral valve ruptures, the blood that must leave the left ventricle towards the aorta artery will return to the left atrium and the lungs.
Hypertensive crisis: a sudden increase in systemic blood pressure makes it very difficult for the left ventricle to expel blood to the rest of the body.
Chronic heart disease: the heart is an organ affected by many diseases, which do not always have a devastating effect on it, but they do deteriorate it little by little. These diseased hearts are usually compensated by natural mechanisms or drugs indicated by the doctor, but situations that require a more excellent functioning of the cardiac pump can cause heart failure. The problems that most frequently produce this effect are physical exercise, increased blood pressure, lack of oxygen in the environment, infection, bleeding, anemia, pregnancy, and hyperthyroidism.
Fluid overload: it is common for patients who need it to be hydrated intravenously in the hospital. An excess of fluid through this route can make it impossible for the heart to mobilize it, and then heart failure occurs.
Non-cardiogenic pulmonary edema
This includes causes that cause fluid invasion of the lungs, but without the heart is diseased. In this case, the problem arises in the blood capillaries’ walls that supply the lungs, as they lose their ability to retain blood inside and allow fluid to pass into the alveoli. The causes are very varied:
Aspiration of gastric juices: in unconscious patients, the cough reflex is diminished, and this causes that, if they vomit, the gastric juices and all the content in the stomach go up to the larynx and go down to the lungs through the trachea. Acids cause damage to the alveolar walls, which allow the liquid to pass through them.
Sepsis: the septic patients are those with such a degree of infection in your body that it is possible to find bacteria or toxins in their blood. These substances cause diffuse inflammation throughout the cardiocirculatory system, causing the arteries to dilate and the capillaries to increase their permeability. In the lung, this has a harmful effect since the veins let fluid pass to the outside.
Trauma: in contusions of the lung, there is direct rupture of the blood vessels, but not only can lung edema occur in this way, but it is also possible that a trauma anywhere in the human body triggers an exaggerated inflammatory response (as happened in sepsis), and substances reach the lung that increases the permeability of the capillaries.
Pneumonia: localized infection in the lungs can have a direct effect on the surrounding capillaries.